Welcome to the first in a two part blog series, focusing on teen diet. We spoke to Abby Ixer, Registered Dietitian, about whether food can positively impact stress, sleep and energy issues in young people, whether teens should take supplements, and common teen nutrient deficiencies.
We hope you enjoy Abby’s article.
Foodwise, the teenage years can be some of the most challenging for children and their parents.
For parents and teens, it’s a time of great change – teens strive for independence to choose their own diet yet often make unhealthy food choices when given freedom of choice, and like many adults, can be influenced by marketing and the choices of their peers.
It can be challenging for a parent to promote independence whilst still ensuring that nutritional needs are met. Many parents struggle to encourage their children to maintain a healthy diet when they reach adolescence – for example there may be healthy options on the school lunch menu but that doesn’t mean that they will be chosen by their kids!
Many issues arise during adolescent years including body image, exam stress, sleep disturbances and difficulty with concentration as the teenage body undergoes numerous hormonal, physical and emotional changes.
Stress and other issues
The British Nutrition Foundation states that eating a healthy, balanced diet and staying active are not only good for overall health, but could also help to cope in times of stress. With exams and peer pressure at the forefront, the teenage years can be a stressful time which sees many children reaching for unhealthy foods for comfort and convenience. Many teenagers are unaware of the impact of an unhealthy diet on their overall wellbeing – not just their weight but also their sleep quality, ability to concentrate, their skin and their mental health.
So, what is a healthy balanced diet for teens?
General healthy eating tips for teenagers:
- Have regular meals – avoid skipping breakfast. Around a third of young people regularly avoid having breakfast on school days. It is a myth that skipping breakfast can aid weight loss, as many teenagers believe. Starting the day with a balanced meal reduces the desire to snack on unhealthy foods later on and maintains energy levels throughout the morning.
- Include a variety of food groups for balance including fruits and vegetables, starchy foods, protein and dairy or alternatives. Encourage teens to get involved with food shopping and cooking. If they have some input into their meals they may be more inclined to try a variety of foods.
- Eat plenty of fruits and vegetables. On average, only 7-10% of children aged 11-18 years consume the recommended five portions of fruits and vegetables daily, meaning that the majority of young people are missing out on vital nutrients.
- Choose healthier snacks – sugary snacks may result in a sugar high and subsequent fatigue later on. Consumption of free sugars should not exceed 5% of a teenager’s total energy intake daily. Free sugars include all sugars added by manufacturers as well as those naturally present in honey, syrups and unsweetened fruit juices. The most recent result from the National Diet and Nutrition Survey (published in April 2018) show that young people’s intake of sugar is way above the recommended levels and only 5% of 11-18 year olds meet this recommendation.
- Drink plenty of fluid to stay hydrated – aim for 6-8 glasses a day (or 1.5-2 litres). Water is the healthiest choice, making up 60-70% if the human body. It is best to avoid too many fizzy drinks and fruit juices due to the high sugar content. Fruit juices should be limited to no more than 150mls daily. Also be wary of smoothies as these can also be high in sugar. Data shows that the main source of sugar in a teenager’s diet comes from non-alcoholic drinks. This is especially important for active teens who participate in a lot of sport. Healthy drinks include water, milk, sugar free squash or herbal tea.
The three vitamins and minerals that your teenage child may need more of:
The main current healthy eating advice for teenagers is based on the Eatwell Guide (see link in references below). However, there are specific micronutrients that are particularly important for teenagers. These include:
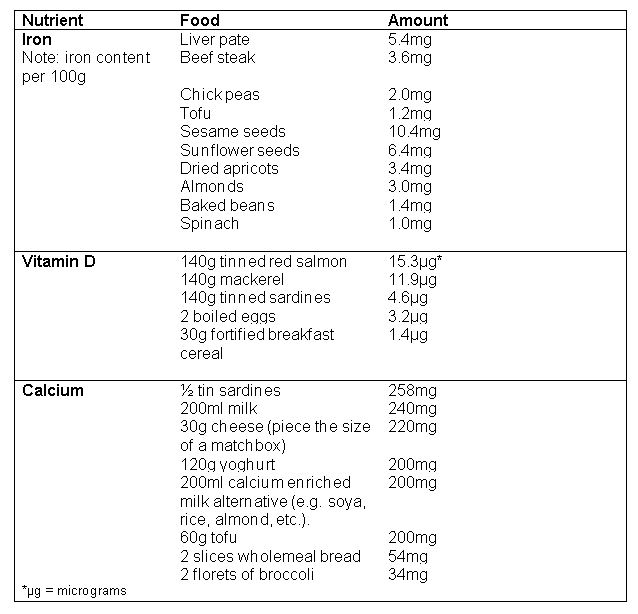
iron:
Iron is essential for building red blood cells to transport oxygen around the body to use for energy. Teenage requirements for iron are higher than any other age group, as their bodies are still growing and preparing them for adulthood. Teenage girls need more than boys (14.8mg for girls compared to 11.3mg for boys). Survey data shows that around 48% of 11-18 year old girls in the UK consume below the recommended amount of iron. Iron deficiency (known as anaemia) can lead to fatigue, lethargy and weakness. Iron rich foods include red meat, green leafy vegetables, dried fruit, nuts, beans, wholegrains and fortified breakfast cereals. Vitamin C helps us to absorb iron, so including fruits or vegetables with each meal will increase the absorption.
vitamin d
Vitamin D is needed to aid the absorption of calcium – essential for the maintenance of healthy bones and teeth. Vitamin D is produced mostly in the skin in response to sunlight, but can also be found in small amounts in oily fish, red meat, eggs and fortified breakfast cereals.
calcium:
Calcium is required to maintain healthy bones and teeth. The majority of bone mass is built in childhood, and by the time our children reach the end of their teenage years, their bones have already almost reached their maximum strength and density. Therefore it is crucial to ensure optimal nutrition during the teenage years in order to ensure healthy bones as adults. Teenagers need more calcium than any other age group; with males needing 1000mg daily and females needing 800mg daily (the average adult needs just 700mg). Calcium can be found in dairy products (milk, cheese, and yoghurt), tinned fish, green leafy vegetables, nuts and soya products (such as tofu).
The following table lists recommended sources of iron, vitamin D and calcium in various common foods.
Does my teenager need a supplement?
According to NHS guidance, if a teenager is eating a balanced diet, they generally shouldn’t need any supplements unless there is a known deficiency.
The exception is vitamin D, as the body is unable to produce vitamin D all year round because sunlight exposure is reduced during the winter months. Generally, the body should produce enough during the summer to maintain good reserves during the colder part of the year. In today’s society, teenagers are spending more time indoors and therefore receiving less sun exposure during the summer and as a result, the incidence of deficiency is increasing. In recent years, low vitamin D status has been observed in 22% of 11-18 year olds across the year as a whole, with an increase in deficiency being observed during the winter months. As there are very few dietary sources of vitamin D, the new government guidance states that teenagers should consider taking a daily 10µg vitamin D supplement during autumn and winter.
meal ideas for optimum teen nutrition:
Whilst we all understand the concept of a balanced diet, it’s easy to get stuck in a rut of the same old breakfasts, lunches and dinners. We asked Abby for some quick meal ideas which to help fuel your teen through the day, and minimise energy slumps.
breakfast
Porridge made with milk (or a dairy free alternative). Try one of these tasty variations:
o ‘Crunch’ porridge: small handful of dried fruit and mixed seeds (try dried apricots and pumpkin or sunflower seeds).
o ‘Apple pie’: grated apple, a small handful of flaked almonds and a pinch of cinnamon.
o ‘Banana bread’: mashed banana, a small handful of pecan buts and a pinch of nutmeg.
o ‘Summer berry’: cooked apple and berry compote
o ‘Carrot cake’: grated carrot, a small handful of walnuts and a pinch of cinnamon.
Wholegrain cereal such as shredded wheat, bran flakes, Special K or Weetabix).
Wholemeal/seeded toast with one of the following:
o Peanut butter
o Marmite
o 2 poached or scrambled eggs
o ½ tin of baked beans
Also include a piece of fruit or 150ml of fruit juice for extra vitamin C and a calcium rich food (e.g. low fat yoghurt, glass of milk, etc.)
lunch:
Jacket potato, baked beans, cheese, salad
Sandwich with various fillings:
o Tuna and cucumber/sweetcorn/green pepper.
o Chicken/turkey, lettuce and tomato.
o Smoked salmon, low fat cream cheese and cucumber.
o Egg and cress.
o Hummous and red pepper.
o Peanut butter and banans
Tinned sardines on wholemeal toast.
Lentil and vegetable soup.
Omelette – add vegetables for a vitamin and fibre boost.
Also serve with a piece of fruit and a calcium rich food as before.
dinner:
Bean chilli or stew served with brown rice/couscous and vegetables.
Spaghetti Bolognese – made with lean beef mince and served with whole-wheat pasta and salad.
Serving of meat/fish/tofu with boiled new potatoes (skins on) and vegetables.
Try to ensure that main meals contain a balance of carbohydrates, protein and vegetables.
snacks:
A handful of mixed nuts and dried fruit.
Low fat Greek yoghurt with fresh fruit.
Carrot/cucumber/pepper sticks with hummous.
Small wholemeal pitta bread with hummous or tahini (sesame seed dip).
Sliced apple with 1 teaspoon of peanut butter.
Oatcakes with low fat cream cheese.
30g piece of cheese and a handful of cherry tomatoes.
Plain popcorn – add a sprinkle or chilli powder or cinnamon for extra flavour.
Glass of milk (or dairy free alternative).
For a sweet treat, try homemade frozen yoghurt - mix together low fat Greek yoghurt with mashed banana and chopped mixed berries. Freeze until solid, stirring occasionally.
Join us for part two (published 19th nov 2018), when we discuss teenagers and caffeine, sleep, memory and stress.
And sign up below for a live teenage diet Q & A with Abby, and Organic Cookery School founder, Lucy, on 25th November 2018 (limited places)
References and further reading:
https://www.nhs.uk/live-well/eat-well/healthy-eating-for-teens/
https://www.bda.uk.com/foodfacts/Diet_Depression.pdf
https://www.bda.uk.com/foodfacts/PackedLunches.pdf
https://www.gov.uk/government/publications/the-eatwell-guide
https://www.gosh.nhs.uk/teenagers/staying-healthy/healthy-eating
https://www.nutrition.org.uk/healthyliving/lifestages/teenagers.html
http://www.ipswichandeastsuffolkccg.nhs.uk/Yourhealth/Youthhealth/Healthyeating.aspx
https://www.nutrition.org.uk/nutritionscience/nutrients-food-and-ingredients/liquids.html?start=1